Buy Ganfort Online
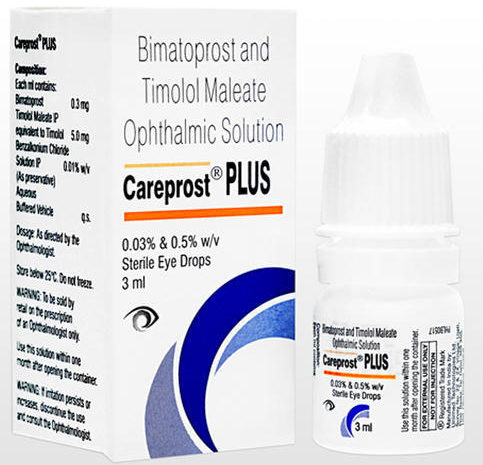
We sell Generic Version of Original Ganfort, under brand name Careprost Plus made by Indian company.
| Active substance: | Bimatoprost + Timolol |
| U.S. Brand: | Ganfort |
| Indian Brand: | Careprost Plus |
| Mfd by: | |
| Strength: | 0.03% + 0.5% w/v |
| Form release: | 3ml bottle |
| Shipping time: | 7 – 21 days |
| Best price: | 12.00 USD |
| Order: | through request form |
Bimatoprost in combination with Timolol is used for treating ocular hypertension (by draining fluid from the eye) or increased pressure in the eye and open-angle glaucoma. It comes in the form of eye drops. Bimatoprost & Timolol released under US brand name: Ganfort, we sell 100% analog/generic brand CAREPROST PLUS is included in a class of medications called prostaglandin analogs, Generic Ganfrort – Careprost Plus made by trusted indian company Sun Pharma.
The drug should be used in the morning. If you miss one dose, continue with the next one.. The eye solution may vary from clear, colorless to slightly yellow in color. The medicine is available in 5 ml white opaque polyethylene bottle. Each bottle contains 3 ml of solution. The bottle should be kept tightly closed. It should be used within 30 days of opening the bottle.
Combination Bimatoprost & Timolol, It is generally advised to be used in the affected eye once daily. Both these drugs work differently to control the increased pressure level in the eye. While using these eye drops, be careful not to touch the tip of the dropper, as it may contaminate the tip as well as the solution. Sometimes, brand or generic Ganfort eye drops may temporarily blur your vision, therefore you are advised not to drive a vehicle or operate machinery for some time after using this drug.
Bimatoprost and timilol maleate may cause your eye color to change, which is completely normal. While you are taking this medication, you should go for regular checkup. This drug may also increase your sensitivity. You should consult your doctor if you have a history of allergies. It is also advised that brand or generic Ganfort eye drops be used cautiously if you have decreased liver or kidney function. You should talk with your doctor if you suffer from closed eye glaucoma.
A bimatoprost sustained-release implant reduced IOP by approximately 30% over 12 weeks in a phase 3 clinical study, according to an Allergan press release.
The multicenter, randomized, masked, parallel-group study, which included 594 subjects with open-angle glaucoma or ocular hypertension, compared the efficacy and safety of two dose strengths of Bimatoprost SR and timolol eye drops used twice daily for up to 20 months. The study showed the majority of patients treated with Bimatoprost SR were potentially able to be treatment-free for 1 year after the last implant was inserted, the release said.
“Considering that as many as 80% of glaucoma patients fail to administer their drops on a regular basis, Bimatoprost SR has the potential to transform the management of glaucoma in millions of patients,” Bill Meury, chief commercial officer at Allergan, said in the release.
The implant was well tolerated in the majority of patients. Additional safety data from this study, as well as results from a second phase 3 study, are expected to be reported in the first half of 2019, and the company expects to file a new drug application with the FDA in the second half of 2019, according to the release.
Background: Poor adherence to treatment is a problem in glaucoma, and patient dissatisfaction with topical glaucoma medication is a barrier to adherence. The objective of this study was to evaluate glaucoma patients’ satisfaction with fixed-combination bimatoprost/timolol ophthalmic solution (BTFC).
Methods: This observational, multicenter study was conducted in China in adults with glaucoma treated with BTFC for 1–3 months. Five hundred patients answered a questionnaire concerning their demographic characteristics, history of glaucoma and topical glaucoma treatment, and use of BTFC. The primary endpoint was patient satisfaction with BTFC assessed on a 10-point scale (1= very dissatisfied, 10= very satisfied).
Results: Patients received BTFC alone (65%) or with other treatments (35%), most commonly a carbonic anhydrase inhibitor. Most patients (87%) used BTFC as a replacement for other medication, usually a β-blocker or prostaglandin analog; 13% received BTFC as add-on treatment. Key reasons for initiating BTFC therapy were poor efficacy of previous treatment (72% of patients) and side effects of previous treatment (32% of patients). Most patients agreed or very much agreed that BTFC provided better control of intraocular pressure (85% of patients), had a simpler administration (87% of patients), and was associated with better tolerance and comfort (82% of patients) compared with their previous treatment. Mean satisfaction scores were significantly higher for BTFC than for previous treatments among all patients (7.8 versus 6.0; P<0.0001) and within patient subgroups based on demographic characteristics, pattern of BTFC use, and previous treatment.
Conclusion: Patients were highly satisfied with BTFC used alone or concomitantly with another topical medication. Patients previously treated with a β-blocker, prostaglandin analog, carbonic anhydrase inhibitor, α-adrenergic agonist, or combination of two medications were more satisfied with BTFC than with their previous treatment. Most reported that intraocular pressure control, tolerability, and ease of administration improved with BTFC.
Keywords: bimatoprost, fixed combination, glaucoma, patient compliance, timolol
Glaucoma is a heterogeneous disease characterized by the development of increased intraocular pressure (IOP) that leads to structural changes and nerve damage within the eye. Manifestations of this disease include chronic progressive open-angle glaucoma (OAG) and acute angle-closure glaucoma (ACG), both of which may be categorized as either primary or secondary, depending on the underlying cause.Glaucoma ranks among the top five causes of moderate to severe visual impairment and is the third leading cause of blindness worldwide.
Global estimates from 2013 suggest that more than 64 million people aged 40 to 80 years have either primary OAG or primary ACG, and with an increasing elderly population, that number is anticipated to reach 76 million by 2020 and 111.8 million by 2040. As ACG is mainly treated through surgery, this review will focus on chronic therapies used to manage OAG.
Patients with OAG often present with an elevated IOP (normal range: 10–21 mmHg), however, a small subset of patients may develop ocular changes with an IOP < 21 mmHg and are referred to as having normal tension glaucoma. Conversely, some patients with an IOP > 21 mmHg do not go on to develop visual impairment and are referred to as having ocular hypertension (OHT). Control of glaucoma focuses on managing the outflow of the eye’s aqueous humor. The primary exit route is via the trabecular meshwork and through the Schlemm’s canal, also known as conventional outflow, while outflow through the ciliary body and suprachoroidal space, known as unconventional or uveoscleral outflow, accounts for a minor amount of outflow. Topical medications represent the first line of treatment, but if IOP control is inadequate, patients may require escalation to laser-based therapies or surgical procedures.
Several classes of medications are available to treat OAG, but the recommended initial therapy is with a medication from either the beta blocker or prostaglandin analog classes.Prostaglandin analogs work by increasing aqueous humor outflow through the uveoscleral pathway. Beta blockers are believed to act by reducing the production of aqueous humor. A brief overview of the various classes of medications and products available in the United States is provided in Table 1. The usual treatment goal is to achieve a 25%–30% reduction from the patient’s baseline IOP, but other factors such as baseline IOP, pre-existing nerve damage, risk for disease progression, or development of adverse effects may prompt providers to pursue more aggressive or lenient therapeutic goals. Patients may require multiple eye drops from different classes in order to achieve the IOP goal.
Despite the number of effective medications and readily available generic and combination products, there remains a need for new and innovative therapies. One key area for improvement is patient adherence. A survey of patients with glaucoma revealed a number of barriers that prevent effective disease management, including difficulty with effective administration of eye drops, poor medication and disease education, and nonadherence with complex dosing regimens.Some treatments discussed below seek to address adherence through the use of innovative delivery methods that prolong medication activity. Physicians also desire therapies with novel mechanisms that are able to lower IOP more effectively and medications that could provide protection against ocular nerve degeneration.Below (and summarized in Table 2) is a brief overview of several new agents, in no particular order, that have recently been approved or are poised to enter the market in the coming years.
Rhopressa (netarsudil ophthalmic solution)
In December of 2017, the Food and Drug Administration (FDA) approved netarsudil, the first of a new class of medications known as Rho kinase (ROCK) inhibitors. In addition to inhibiting ROCK, this medication also possesses other IOP-lowering mechanisms, such as the inhibition of norepinephrine transport and an ability to reduce episcleral venous pressure. The double-blind, randomized, multicenter trial ROCKET-1 (N=411) compared the efficacy of netarsudil 0.02% dosed once daily at nighttime with timolol maleate 0.5% dosed twice daily. The ROCKET-2 trial (N=756) had a similar design, with an additional netarsudil 0.02% twice-daily dosing arm. Both trials followed patients with OHT or OAG who had an IOP of > 20 mmHg and < 27 mmHg for three months. The primary endpoint in both trials was a reduction in IOP. In ROCKET-1, patients with a baseline IOP < 27 mmHg who received netarsudil demonstrated a 15%–22% reduction in IOP as compared with a 17%–22% reduction in patients who received timolol, but this was not sufficient to demonstrate noninferiority based on prespecified criteria. A post-hoc analysis that focused on patients whose baseline IOP was < 25 mmHg was able to demonstrate noninferiority.
ROCKET-2’s primary efficacy population focused on patients with an IOP < 25 mmHg and was able to demonstrate mean reductions of 3.3–4.6 mmHg and 4.1–5.4 mmHg in patients receiving daily and twice-daily netarsudil, respectively. These reductions were similar to those seen with twice-daily timolol, which produced a 3.7–5.1 mmHg reduction from baseline and demonstrated the noninferiority of netarsudil. In terms of percent reduction in IOP, daily netarsudil was able to achieve a 16%–21% reduction, while twice-daily dosing showed a 22%–24% reduction; twice-daily timolol demonstrated an 18%–23% reduction.
The use of netarsudil appears to be generally well tolerated, with the most common observed adverse effect being conjunctival hyperemia (50%–53%), followed by conjunctival hemorrhage (13%–15%), and cornea verticillata (5%–9%). Other adverse effects including blurred vision, eye pain or erythema, and erythema of the eyelid, were also noted in > 5% of patients.Aerie Pharmaceuticals also conducted the ROCKET-4 trial to demonstrate the six-month safety of netarsudil. Results from this trial, released in April 2017, showed daily netarsudil to be non-inferior to twice-daily timolol. The frequency and severity of effects were seen at similar rates to those in the ROCKET-1 and ROCKET-2 trials.
The entry of netarsudil into the market is exciting as it is a novel, well tolerated, once-daily agent. One limiting factor to this medication is its reduced efficacy in patients with a baseline IOP of 26 mmHg or higher. As Aerie Pharmaceuticals has already obtained approval in the United States, it is anticipated to launch in 2019 in the European Union and in 2021 in Japan.
Roclatan (netarsudil/latanoprost ophthalmic solution)
Roclatan, a combination product containing netarsudil and the prostaglandin analog latanoprost, is also being developed by Aerie Pharmaceuticals. This fixed-dose combination would be administered as a once-daily eye drop in the evening and is formulated as a netarsudil/latanoprost 0.02%/0.005% solution. The IOP-lowering effects of netarsudil are expected to be complemented by increased outflow by way of the uveoscleral pathway, facilitated by latanoprost.
The Mercury 1 trial randomized 718 subjects into three treatment arms: netarsudil monotherapy, latanoprost monotherapy, or netarsudil/latanoprost combination therapy, each dosed once daily. The primary efficacy outcome was mean IOP at three months; patients were observed for 12 months for ocular and systemic safety outcomes. At 90 days, patients who received the combination therapy achieved 1.3–2.5 mmHg lower mean IOP than patients who received latanoprost monotherapy, and 1.8–3.0 mmHg lower mean IOP than patients who received netarsudil monotherapy. Significantly more subjects receiving combination therapy demonstrated a 20% or greater IOP reduction and achieved an IOP of < 18 mmHg. While no serious adverse events were reported, a higher percentage of patients discontinued therapy at three months in the combination (15.5%) and netarsudil monotherapy (17.6%) arms versus latanoprost monotherapy (5.5%), with adverse effects being cited as the most common reason for discontinuation. Conjunctival hyperemia was reported in approximately 50% of patients, with most cases being described as mild. Approximately 5% to 11% of patients reported experiencing conjunctival hemorrhage, pruritus, increased lacrimation, and cornea verticillata.
The Mercury 2 trial evaluated changes in IOP at 90 days in 750 participants receiving netarsudil/latanoprost, netarsudil monotherapy, or latanoprost monotherapy. Similar to the Mercury 1 findings, the combination agent was able to lower IOP an additional 1.5–2.4 mmHg compared with latanoprost monotherapy and an additional 2.2–3.3 mmHg when compared with netarsudil monotherapy. Fifty-six percent of patients receiving netarsudil/latanoprost were able to achieve a diurnal IOP of < 16 mmHg.
An additional clinical trial (Mercury 3) is underway to compare the safety and efficacy of netarsudil/latanoprost with that of the combination bimatoprost/timolol 0.03%/0.5%. This trial, which is still recruiting patients, will aim to enroll 472 participants and evaluate changes in IOP at six months in addition to clinical safety endpoints. Currently, no additional information is available regarding this study, but the anticipated completion date is April 2019. Aerie Pharmaceuticals filed a New Drug Application on May 15, 2018 and expects a decision from the FDA within 10 months.
OTX–TP
Ocular Therapeutix is developing a bio-resorbable canalicular implant that will continuously deliver the prostaglandin analog travoprost for up to 90 days. The active medication is encapsulated in a biodegradable polyethylene-glycol hydrogel that will swell upon implantation to retain its position in the eye. This plug is inserted through noninvasive methods by a specialist and does not require removal as it exits through the nasolacrimal system.This novel delivery system addresses the major issue of poor patient adherence and is poised to be the first of several implantable therapies to enter the major markets.
A phase 2b study evaluated efficacy and safety of a punctum plug of travoprost against timolol maleate 0.5% drops twice daily in 79 patients. Participants were enrolled if they had a diagnosis of OHT or OAG with a mean baseline IOP of ≥ 24 mmHg at Hour 0 and an IOP of ≥ 22 mmHg when checked 4 and 8 hours later. Mean reductions in IOP were evaluated at 30, 60, and 90 days at multiple times each day (8 a.m., 12 p.m., and 4 p.m.). Patients in both groups demonstrated a reduction in IOP from baseline, although those receiving OTX–TP showed a 3.27–3.54 mmHg reduction while those receiving timolol experienced a 5.84–6.29 mmHg reduction. These reductions in IOP were observed at all time points throughout the day. The reported rates of ocular (39.4% vs. 37.5%) and non-ocular (9.1% vs. 7.5%) adverse effects were similar in the OTX–TP and timolol arms, respectively. The most common adverse effects were dacryocanaliculitis (12.1% vs. 10%), acquired dacryostenosis (6.1% vs. 5%), eyelid edema (6.1% vs. 0%) and scar (6.1% vs. 0%) in the OTX–TP and timolol groups, respectively.
Ocular Therapeutix is now enrolling patients for a phase 3, placebo-controlled trial evaluating the efficacy and safety of OTX–TP in the treatment of OAG or OHT. This trial will aim to enroll 550 patients with a primary endpoint of changes in IOP at Weeks 2, 6, and 12, at 8 a.m., 10 a.m., and 4 p.m. Ocular Therapeutix expects to complete this trial in December 2018.While OTX–TP has the advantage of a noninvasive route of administration and is likely to be the first long-acting implant to enter the market, the lower impact on IOP as compared with timolol drops observed in the phase 2b trial and lack of active control in the upcoming phase 3 trial may make some providers unsure of its place in therapy.
Bimatoprost Sustained-Release Ocular Implant
Allergan is reformulating its prostaglandin analog, bimatoprost, into a sustained-release ocular implant as a way to enhance patient adherence. Bimatoprost SR would continuously deliver medication over six months after being inserted via injection into the anterior chamber of the eye through a noninvasive procedure.
A phase 1/2 prospective, dose-ranging trial that examined 75 patients with OAG demonstrated a rapid and sustained lowering of IOP with bimatoprost SR. Following a washout period, enrollees intracamerally received various doses in the study eye while the other eye was treated with topical bimatoprost 0.03%. Overall mean IOP reductions of 7.2, 7.4, 8.1, and 9.5 mmHg were seen in patients receiving 6, 10, 15, and 20 mcg of bimatoprost SR, respectively, as compared with an 8.4 mmHg reduction with topical bimatoprost. Patients initially reported higher rates of adverse effects such as eye pain, foreign body sensation in the eye, and conjunctival hemorrhage with bimatoprost SR but these symptoms subsided within two days of onset. Following Day 2, the eye receiving bimatoprost SR had less reported conjunctival hyperemia (6.7% vs. 17.3%) than the eye receiving topical bimatoprost, while reports of other adverse effects remained similar between the eyes. When questioned at Day 8, 79.7% of patients reported the procedure to be less burdensome than anticipated and, at Week 12, 77% of patients were very or extremely likely to have another implant procedure.
An ongoing phase 3 trial enrolling 594 patients with OAG or OHT is comparing twice-daily timolol drops to two undisclosed doses of bimatoprost SR administered on Day 1, at Week 16, and at Week 32. The primary outcome will be changes in IOP from baseline to Week 12; however, patients will continue to be followed for a 12-month treatment duration plus an additional eight-month extended follow-up.A second trial, similarly designed, is aiming to enroll 600 patients and has an estimated primary completion date of March 2019. Two additional trials are comparing bimatoprost SR with selective laser trabeculoplasty in patients with OAG or OHT who are unable to be controlled with topical IOP-lowering therapies. In these trials, an undisclosed dose of bimatoprost SR will be administered on Day 1, at Week 16, and at Week 32. The primary outcome will be changes in IOP at Week 24. Investigators seek to enroll 160 patients for each study and have estimated primary completion dates of November 2019 and May 2020.
DE-117
Santen Pharmaceutical is developing a novel agent that acts on a new target in the prostaglandin pathway, the prostaglandin EP2 receptor. While other prostaglandin analogs bind to the F2-alpha receptor, DE-117 activates the EP2 receptor and is thought to lower IOP by regulating outflow through the conventional pathways. This novel mechanism may position DE-117 to be a viable option in patients for whom other prostaglandin analogs have not adequately lowered IOP. In November 2017, Santen filed for approval of DE-117 in Japan while continuing to conduct trials in other markets. There are several clinical trials involving DE-117 for which enrollment is complete but results have not yet been posted.
Among these trials: The phase 2 SEE-1 trial, evaluating five doses of DE-117 against latanoprost among 184 participants in several centers across the United States, was listed as having completed enrollment as of April 2018; a long-term, open-label trial known as RENGE, involving 125 patients and that compared two groups of DE-117 monotherapy with patients receiving the combination DE-117 and timolol ophthalmic solution, was listed as having been completed in November 2017, and the AYAME study, which also evaluated two doses of DE-117 against a placebo arm as well as a latanoprost arm in 253 patients with OAG and OHT.
One trial for which results are available evaluated four varying concentrations of DE-117 against placebo and latanoprost in 91 patients. At the end of 4 weeks, investigators found that a concentration of 0.002% of DE-117 performed the best and matched the IOP-lowering effect of latanoprost. The most commonly observed adverse effects in the 0.002% dosing arm, all seen in approximately 14% of patients, included conjunctival and ocular hyperemia, photophobia, and eye pain.28 The only trial listed as recruiting patients is a phase 3 trial comparing DE-117 directly to latanoprost in patients with OAG or OHT in an anticipated 360 patients. The primary outcome is mean diurnal IOP at three months, and the expected completion date is November 2018.
CONCLUSION
Several other long-acting formulations of established medications are in the early stages of development, which suggests that addressing the issue of poor patient adherence is an area of keen interest. In addition, new medications belonging to established classes, such as prostaglandin analogs, are in early development, as are new therapeutic classes such as guanylate cyclase activators. With these novel treatment options on the horizon, better management of glaucoma looks promising for the near future.
Submit your review | |
1 2 3 4 5 | |
Submit Cancel | |